If you came out of this holiday season feeling mad as a hatter, you aren’t alone. Although your madness was likely secondary to family time, while the hatters of the 18th century went mad due to mercury exposure, but both exposures can be potent.
While risk of heavy metal exposures are generally low, you will likely face questions about metal exposure at some point in your career (i.e. What types of fish should your pregnant patients eat? Should people with mercury dental fillings have them removed? Does your patient need to test their well water for arsenic?) This newsletter is designed to give you all the information you need to know about heavy metals (the elemental kind, although Linkin Park is also on tour if you need a little aural metal adjacent content in your life).
A 30-year-old female patient comes to see you with her husband for a preconception visit. You make sure she is up to date on annual screenings, discuss genetic screening and put her on a prenatal vitamin. Her husband has recently gotten into herbalism and has been reading about the ways different foods and substances may affect their future child. He discloses that your patient likes to eat a tuna sandwich for lunch a few days out of the week. He is trying to convince her that eating fish during pregnancy is not good for the baby. Additionally, he has done some reading about metals used in dental fillings, and he is concerned that their future child may have increased risk for cognitive impairment due to the fillings his wife had placed a few years ago.
These questions come up in clinical practice and require a little knowledge of mercury toxicity to address. So, let’s dive into the mercurial waters of this heavy metal.
Mercury
Mercury exposure may lead to CNS injury, hepatotoxicity, GI ulcers, and renal dysfunction. The mechanism of mercury toxicity includes reactive oxygen species production, glutathione bonding, increased c-fos (proto-oncogene) expression, and damage to the proximal renal tubules. There are two main forms of mercury that exert different health effects, methylmercury, and metallic mercury. Metallic mercury is turned into methylmercury by bacterial processes and is the compound that accumulates in the food chain.
Health effects of methylmercury include:
loss of peripheral vision
changes in coordination
muscle weakness
numbness
difficulty walking
speech and hearing impairment
Methylmercury is a neurotoxin, and can impact cognition, memory, attention, language and motor skills of children when they are exposed in utero. Elemental mercury exposure occurs when breathing in mercury after a spill or when a product containing mercury breaks; exposures to elemental mercury are less common due to the decreasing prevalence of mercury in common household products. If exposed, elemental mercury can cause CNS changes, as well as affect the renal and respiratory systems. Due to these deleterious health effects, the EPA has recommended a blood mercury concentration of 5.8 mcg/L or less as likely to be safe. The CDC and ATSDR consider the toxicity data not yet clear enough to establish a safe level.
Fish:
The mercury conversation almost always involves fish, so we will spend the most time discussing guidelines for fish consumption (which are quite simple).
The groups who should be most cautious about mercury exposure are pregnant folks, those thinking of becoming pregnant, and children between the ages of 1-11. Luckily the FDA made a special guide just for these groups!
Takeaway point for pregnant folks:
It is recommended to eat 2-3 servings of low mercury fish weekly (see below). For reference, 1 serving is the size of your palm.
Compounds such as iodine, omega 3, omega 6, choline and iron are all found in high concentrations in fish and are important for in utero neural development.
When thinking about a fish and its mercury content, you want to eat lower on the food chain, as bigger fish eat smaller fish which results in bioaccumulation of mercury. Farmed fish generally have lower levels of mercury than wild fish, although this is variable depending on the farming conditions.
Tuna is always the big fish in the room and a significant source of mercury. Pole caught tuna is best (since the fish is smaller). Skipjack (often called light tuna when canned) is the best species due to lower mercury and high selenium levels (it’s also a smaller tuna species, so lower on the food chain). Its conservation status is “least concern” which also makes it a better option from a biodiversity standpoint (although we will leave ethical questions about the fishing industry out of today’s newsletter). Yellowfin is a good second option, but try to avoid Bigeye and Albacore (often called white) tuna if you can. If possible, try not eat tuna more than a few times a month.
As you can see in the chart below, most other common fish are safe for consumption, including tilapia, whitefish, salmon, flounder, cod and catfish! So, get fishy to your heart’s content (i.e. up to 2-3 times per week especially if pregnant).
Subsistence fishing is more common than we might think and is an protein for individuals with limited resources. If someone plans to eat fish that they or their family have caught, have them check local fish advisories and become familiar with how to determine the safety of locally caught fish and seafood.
Other Routes of Mercury Exposure to Consider:
- Consumer products such as old appliances, thermometers, barometers, thermostats. See here for a comprehensive list.
- Dental amalgams (fillings) often contain liquid mercury. Whether or not these are bad for us has been a hot topic since before the founding of the American Dental Association. However, numerous studies have shown that exposure from amalgams (via mercury vapor released when eating) does not result in significant increases in blood mercury levels.
People with multiple dental amalgams or amalgams that are in poor condition have higher blood levels of mercury.
So far, there is no evidence that they have detrimental effects on health in otherwise healthy individuals, or that removing them has any health benefit (removal of dental amalgams was a concerning trend in past years).
However, people with neurologic or renal disease should have blood mercury levels drawn and if elevated consider the role of amalgams.
-Mercury can also be used in gold mining, so if you ever see a gold miner from abroad come to see you in your office, rack up some real zebra bonus points by diagnosing neuropathy secondary to mercury exposure.
You are working on an Indian Health Service site in the Southwest. A family comes in to discuss skin changes they have noticed. The mother notes that her whole family has developed dark spots on their palms. Additionally, her youngest two children have had waxing and waning numbness and tingling in their lower extremities. On exam there are no abnormalities except for multiple, firm, symmetric discolored nodules on their hands, and two of the children have scattered hypopigmented macules on their upper extremities (pictured below). They recently moved to a more remote location. Upon further questioning you learn that they have their own well on the property that they use for drinking water. What do you want to do next?
This case is meant to highlight some of the symptoms of arsenic exposure. The short answer to this case is that you would want to have them test their well water for arsenic and other heavy metals. Additionally, you could test their individual levels of arsenic through a spot urine test. If you do test arsenic levels in a patient, make sure they have abstained from eating any fish or any other seafood for a few days before the test (you’ll find out why below).
Arsenic
Arsenic is not just a poison used in spy movies and historical events (some think Napoleon died of arsenic poisoning) and it hangs around more places than you’d think. Arsenic is commonly found in the earth’s crust, and levels of arsenic are often higher in areas with rocky, dusty terrain. It can bioaccumulate in the food chain, although this occurs in its organic form arsenobetaine which is less harmful and not known to be toxic to humans.
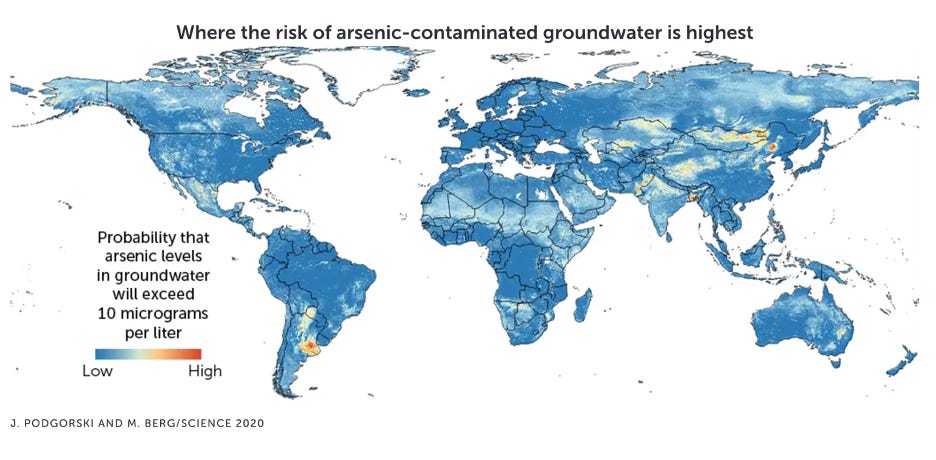
Arsenic is the most significant chemical contaminant in drinking water globally (some estimate 220 million people are exposed to unsafe levels of arsenic in drinking water on a daily basis), and its less toxic, organic form can be found in many different types of seafood (which is not thought to have any negative health effects, but will be detected on an arsenic urine test. The right test to order is Arsenic, Urine with reflex to fractionated. This test will differentiate the toxic inorganic from the less toxic organic forms of arsenic) ). The WHO and EPA both have limits for arsenic in drinking water set at 10 μg/L, although as you can see below, many areas of the country exceed this measurement.
Geographic Representation of Arsenic and Uranium in Community Water Systems (CWS)
In the acute setting, exposure to arsenic leads to GI distress, numbness and tingling, muscle cramping and in extreme circumstances, death. Chronic exposure to arsenic can lead to changes in skin pigmentation, as well as skin, lung and bladder cancer. Exposure in utero and in young children leads to increased mortality, multiple cancers, kidney failure, heart attacks and respiratory disease. Additionally, when exposed early in life, arsenic is a neurotoxicant, leading to decreases in memory, cognitive development, and IQ.
For purposes of in office exposure assessment and counseling, we recommended discussing water sources. If you are practicing in an area with higher risk of arsenic exposure, it is beneficial to ask if your patients get their water from a well. If so, they should have that well tested for arsenic.
Uranium: Like arsenic, uranium can be found in dust and rock and can leech into groundwater. The main health effect of uranium is kidney damage, although animal models suggest there may be other health effects. The safe drinking concentration is thought to be 30 mcg/L. I wanted to briefly highlight uranium here due to the disproportionate exposure of Native American communities to uranium due to uranium mines and atomic bomb test sites. 96% of all defense-related uranium mines were on tribal land. Additionally, many tribes in Nevada have continued to be exposed to high levels of radiation due to proximity to atomic bomb testing sites in additional to uranium mines. Studies in that area of Nevada have shown increased incidence of thyroid neoplasms in the areas surrounding the nuclear testing site (although the studies are very small due to the small resident population). The EPA notes that due to uranium mining (until 1970) and nuclear testing (until 1992) “Native American and Alaska Native communities are deeply impacted by contaminated soil, air, water and materials that were left behind” after these events.
A 45-year-old patient presents to your office after recently watching a 60 minutes special on legacy pollution of heavy metals in soil and water. He is concerned that he could have high levels of heavy metals in his blood after growing up in eastern Pennsylvania around many abandoned factories and industrial plants. He lives in Philadelphia in a brand new apartment complex, works as an accountant for the postal service, has no chronic medical conditions, takes no medications or supplements, has no physical or mental concerns, doesn’t drink alcohol, and smokes 1 pack of cigarettes daily.
To wrap up this marathon, I briefly wanted to touch on Cadmium, mostly because it has a cool name, but also because it is perhaps the most likely exposure you will encounter. While acute cadmium toxicity is rare (but discussed below), the tobacco plant naturally has large amounts of cadmium. Thus, tobacco smoke (from processed or hand rolled tobacco) is a risk factor for cadmium toxicity.
Outside of smoking, this patient is not at risk for any other heavy metal exposure (even if he was when growing up, since he is removed from the potential site of exposure, we would not need to test him for anything). However, he is at risk for cadmium exposure due to smoking. Testing his blood cadmium level would be a total waste of time, but by knowing a little bit about cadmium’s effects on the body, you will have one extra tool (that most folks who smoke have not encountered) in your smoking cessation tool belt.
Cadmium
Cadmium exposure has been shown to cause degenerative bone disease, kidney dysfunction (tubular proteinuria), liver damage, lung disorders, deficiencies of zinc and copper. Additionally, it may give rise to kidney, lung, pancreatic, breast, prostate, and GI cancers. The mechanism of cadmium toxicity involves miRNA dysregulation, apoptosis, endoplasmic reticulum stress, lowering PTH, reactive oxygen species generation and dysregulation of calcium, zinc, and iron homeostasis.
Cadmium exposure occurs via consumption of contaminated food or water, inhalation of cigarette smoke, or occupational exposure due to welding or smelting. Of note, there are not many functioning smelters left, however the locations of once-functioning smelters have extensive ground and water pollution (like this town in Eastern Pennsylvania). Cadmium is a potent carcinogen due to its ability to inhibit DNA repair. Outside of its carcinogenic potency, clinical manifestations of cadmium exposure include GI upset when consumed, pulmonary edema, chemical pneumonitis and bronchitis when inhaled. If you have a patient you suspect was exposed to Cadmium you can get a cadmium blood test (expected level up to 1.2ug/L and in smokers up to 3.9 micrograms/L). There is no safe level since it is a carcinogen.
And with that, we have finished our whirlwind tour of heavy metals. As always, send us any questions, topic you’d like us to cover in the future, and please share this newsletter!
Reviewer: Marilyn V. Howarth, MD, FACOEM, Center of Excellence in Environmental Toxicology
Supported by the National Institute of Environmental Health Sciences (Grant number: P 30 ES013508)
References:
- Balali-Mood M, Naseri K, Tahergorabi Z, Khazdair MR, Sadeghi M. Toxic Mechanisms of Five Heavy Metals: Mercury, Lead, Chromium, Cadmium, and Arsenic. Front Pharmacol. 2021 Apr 13;12:643972.
- United States Environmental Protection Agency [Internet]. 2024. Health Effects of Exposures to Mercury. Available from: https://www.epa.gov/mercury/health-effects-exposures-mercury
- World Health Organization [Internet]. 2022. Arsenic. Available from: https://www.who.int/news-room/fact-sheets/detail/arsenic#:~:text=Long%2Dterm%20exposure%20to%20arsenic,increased%20deaths%20in%20young%20adults.
- Farzan SF, Karagas MR, Chen Y. In utero and early life arsenic exposure in relation to long-term health and disease. Toxicology and Applied Pharmacology. 2013 Oct;272(2):384–90.
- Tolins M, Ruchirawat M, Landrigan P. The Developmental Neurotoxicity of Arsenic: Cognitive and Behavioral Consequences of Early Life Exposure. Annals of Global Health. 2014 Nov 25;80(4):303.
- Genchi G, Sinicropi MS, Lauria G, Carocci A, Catalano A. The Effects of Cadmium Toxicity. IJERPH. 2020 May 26;17(11):3782.
- Center for Disease Control: Agency for toxic substances and disease registry [Internet]. 2023. What Health Effects Are Associated With Acute High-Dose Cadmium Exposure? Available from: https://www.atsdr.cdc.gov/csem/cadmium/Acute-Effects.html
- https://www.goodenergycollective.org/policy/the-legacy-of-uranium-mining-on-us-tribal-lands
- https://sgs.princeton.edu/news-announcements/news-2023-07-21
- https://www.epa.gov/radtown/radtown-uranium-activity-5-radiation-contamination-and-exposure
- https://academic.oup.com/toxsci/article/184/1/104/6359195
-Yin L, Lin S, Summers AO, Roper V, Campen MJ, Yu X. Children with Amalgam Dental Restorations Have Significantly Elevated Blood and Urine Mercury Levels. Toxicol Sci. 2021 Oct 27;184(1):104-126. doi: 10.1093/toxsci/kfab108. Erratum in: Toxicol Sci. 2022 Feb 28;186(1):174. doi: 10.1093/toxsci/kfab156. PMID: 34453845.
- Guo, J., Cao, W., Lang, G., Sun, Q., Nan, T., Li, X., Ren, Y., & Li, Z. (2024). Worldwide Distribution, Health Risk, Treatment Technology, and Development Tendency of Geogenic High-Arsenic Groundwater. Water, 16(3), 478. https://doi.org/10.3390/w16030478